Transforming the health visiting service after COVID-19

Parents told us they didn’t know what to expect from the health visiting service. They reported having limited information and said that the service wasn't responsive. During the COVID-19 pandemic, some mums had no contact with a health visitor at all.
Parents who had been seen by a health visitor said they wanted to spend more time discussing their mental health and the types of support available. We heard from 118 people in total, and raised these issue with Sirona care & health, the local provider of the health visiting service, and with their partners in the Community Children’s Health Partnership.
Our recommendations
- Ensure that there is mandatory training in mental health for health visitors so that they feel confident discussing mental health conditions.
- Take steps to standardise and normalise the signposting and recording of support for women with existing mental health conditions.
- Have a process to check mother’s engagement with support for mental health.
- Health visitors help to build awareness of the local Maternity Voices Partnership.
- Make postnatal handovers from the maternity staff to the health visiting service effective and supportive.
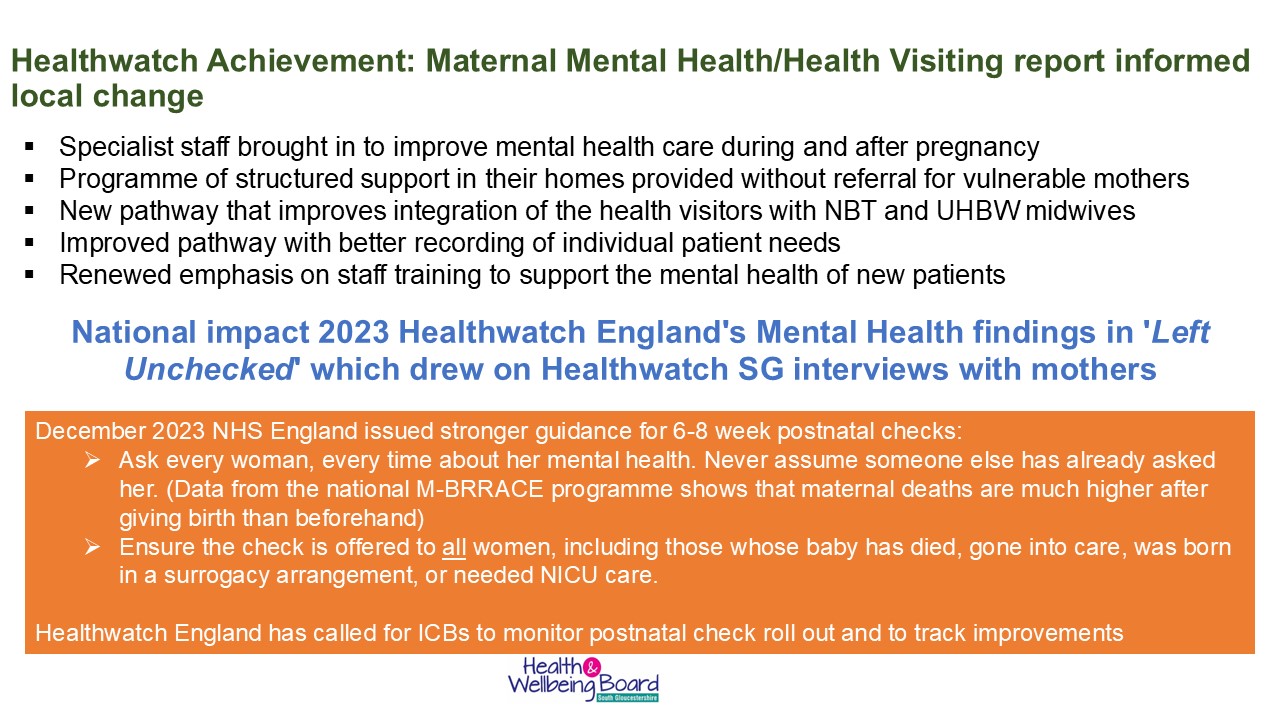
What difference have these findings made?
Health visitors employed to look at perinatal and infant mental health across the local area have brought in specialists who have acted on our insights.This includes provided training to public health nursing staff, supporting the parent-infant relationship, and helping staff with their holistic assessments and support skills, patient referrals, patient signposting and record keeping.
The Healthwatch report for South Gloucestershire contributed a valuable insight which has informed approaches to staff training and liaison pathways.
This team undertook scoping and audits of two areas that our report had pinpointed.
- Improving the pathways for patients into mental health support. There is now renewed importance given to asking mental health assessment questions, to fully support families experiencing challenges with their emotional wellbeing or mental health. The Sirona team audited the standard of the assessment questions, and an updated pathway has now been introduced.
- Improving health visitor practice with families and other professionals has led to better training opportunities, better referrals and a more joined-up approach with midwifery and the third sector. Our report findings aim to influence the mental health workstream for the new family hubs and 'Start for Life' programme, and work on a Bristol, North Somerset and South Gloucestershire-wide perinatal and infant mental health multi-agency pathway.